Hiatal Hernia
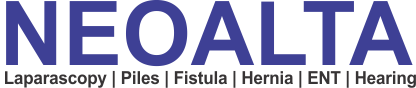
However, patients that have a hiatal hernia have an enlarged opening. A hiatal, or diaphragmatic, hernia occurs when the lower part of the esophagus and a portion of the stomach slide up through this esophageal hiatus into chest cavity.
Sliding Hiatal Hernias
The lower esophageal sphincter at the junction of the stomach and esophagus fails and allows stomach contents to reflux into the esophagus.
The junction may reside permanently in the chest, but often it juts into the chest only during a swallow. When the swallow is finished, the herniated part of the stomach falls back into the abdomen.
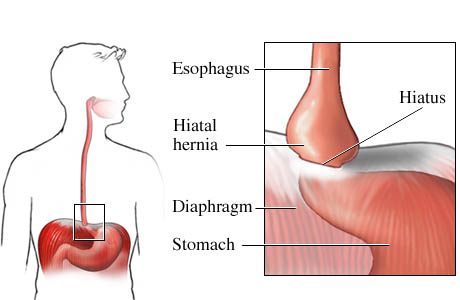
Paraesophageal Hiatal Hernias
The para - esophageal hernias themselves remain in the chest at all times and are not affected by swallows.
Symptoms:
The symptoms associated with the hiatal hernia are variable but generally include:
Surgery: Nissen Fundoplication

In a laparoscopic Fundoplication, small (1 cm) incisions are made in the abdomen, through which instruments and a fiber optic camera are passed.
The operation is performed using these small instruments while the surgeon watches the image on a video monitor. Laparoscopic Fundoplication results in less pain and shorter hospitalization and early return to activities within 2-7 days compared to 4-6 weeks with an open approach.
The stomach and lower esophagus are placed back into the abdominal cavity. Operation may require separation of abdominal organs from the lung and middle chest structures.
Hernia defects greater than 5 cm. are buttressed with mesh which significantly decreases the recurrence rate.
The opening in the diaphragm (hiatus) is tightened and the stomach is stitched in position to prevent reflux.
The upper part of the stomach (fundus) may be wrapped around the esophagus (Fundoplication) to reduce reflux.
The procedure may last for two to four hours depending on the size and contents of the hernia.
-
Chest X-ray:
-
Air fluid level in the chest
-
-
Esophagogram (Barium UGI): Useful in-
-
Assessing the function of the esophagus
-
Identifying structural abnormalities (twisting of the stomach)
-
Associated problems (e.g. aspiration, poor gastric emptying)
-
-
Upper GI Endoscopy (EGD):
-
Identify damage caused by reflux (e.g. esophagitis, Barrett’s esophagus, malignancy)
-
Biopsy esophagus for evaluation of malignancy
-
Esophageal Manometry
-
Assess the function of the LES
-
Assess the propulsive function of the esophagus
-
Our Specialist

Dr. Nitish Jhawar
M.S., FMAS, FIAGES, FALS, FACRSI
Fellow Advance Laparoscopic Surgery
Fellow Colorectal Surgery USA
Senior Laparoscopic & Colorectal Surgeon
Phone No: +91 9322 229 159
Email Id: info@neoalta.com